International Nurses Day 2020: Case study of the week

World Hepatitis Day: Nurse-led hepatitis C clinic, Melbourne, Australia
Contributor: Lilee Foo
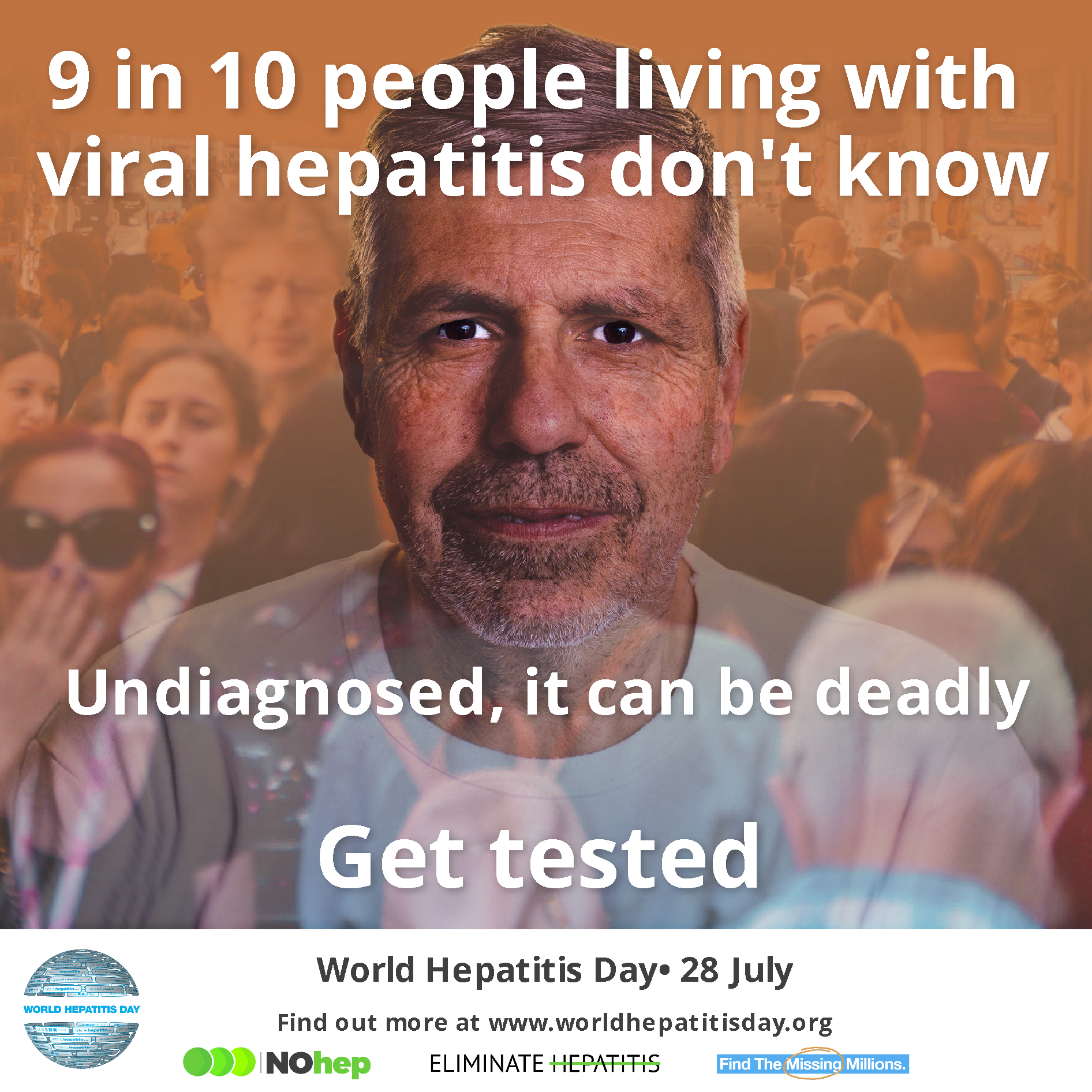
Worldwide, 290 million people are unaware they are living with viral hepatis. Without finding the undiagnosed and linking them to care, millions will continue to suffer, and lives will be lost. That is why the theme for this year’s World Hepatitis Day, 28 July, is “Find the Missing Millions”. To mark this day, ICN brings you this case study from Australia about a nurse-led clinic providing easy access to care for those living with hepatitis C.
The Community Liver Education Assessment and Review service (CLEAR) is a nurse-led clinic that is open for half a day every two weeks. It provides a free and confidential service to people living with hepatitis C in the Box Hill suburb of Melbourne. It is a partnership between Eastern Health (a tertiary hospital) and Carrington Health (a community health service).
The CLEAR service was set up in response to the 2017 listing of new direct-acting antiviral medicines on the Pharmaceutical Benefits Scheme, which is Australia’s government-subsidised prescription drug scheme.
The name was chosen deliberately to avoid any association with hepatitis C, which may have deterred patients because of the stigma associated with the disease.
The clinic provides accessible, timely and appropriate treatment to people with hepatitis C, supports clients to access new treatment (where appropriate), and helps to prevent further complications and disease progression.
CLEAR has links to local pathology services and a gastroenterologist, which, along with support from the Carrington health management team, have been crucial to its success.
Registered nurse Lilee Foo led the clinic and made links with potential referral agencies, including correctional health and local drug and alcohol services. She also liaised with external health services that would provide the necessary pathology, radiology, and general practitioner services, and developed the clinical pathways outlining the appropriate sequence of clinical interventions, timeframes, milestones and expected outcomes for patients.
CLEAR was set up with support funding from the Australian Primary Health Care Nurses Association, and it is now funded through the Medicare Benefits Schedule, Australia’s government-subsidised healthcare scheme, and by funding received by Carrington Health.
The clinic is staffed by an experienced registered nurse employed by Carrington Health and a gastroenterologist employed by Eastern Health, co-located at Carrington Health.
Ms Foo has built her skills and knowledge in relation to hepatitis C with support from Eastern Health liver clinic’s nurse educator and has developed an excellent relationship with Eastern Health’s clinical nurse specialist, which has been key to receiving referrals.
The clinic uses best practice guidelines including those from the Australasian Society for HIV, Viral Hepatitis and Sexual Health Medicine resources and the Australian Department of Health’s National Hepatitis C Strategy.
CLEAR’s model of care was developed based on the experience of established clinics: for example, its assessment form based on one from Eastern Health’s nurse-led clinic in Healesville.
A vital aspect of the programme is that it is patient-centred, holistic and easy to access. All patients undergo a holistic assessment, patient education is tailored to their specific needs and patients are referred on to other services, as needed.
Carrington Health already provides a number of services to at-risk community members, including people who use drugs and alcohol. The CLEAR service was set up because it was anticipated that this cohort of vulnerable patients would be easier to engage in a community setting, rather than a hospital environment.
There are numerous referral points to CLEAR, including:
- Carrington Health’s needle and syringe program
- Self-referral, potential patients can drop in to reception or phone
- A formal referral from a GP
- Primary health care services, including as drug and alcohol services and correctional health
The clinic has adopted processes and systems that are already in place at Carrington Health’s services, including safety, confidentiality and booking appointments, and our reception staff are a key access point for patients to the clinic.
The clinic model has been adapted and modified over time to assist in meeting the needs of the people who attend, and the partnership with Eastern Health.
Usually the patient is assessed by the nurse before they see the gastroenterologist, and sometimes they may perform the assessment together. Generally, patients are followed up by phone or at Carrington Health if that suits them better.
Being flexible and placing an emphasis on engaging and developing a rapport with patients has been important in increasing access to care for those attending the clinic.
Ms Foo is allocated dedicated administration time to ensure that she is able to enter client details into Carrington Health’s medical records software and follow up on other administrative tasks.
The clinic uses Carrington Health’s quality improvement systems, including feedback forms at reception, and the increasing number of enquiries received is an indicator that the clinic is acceptable and accessible to patients.