WHO DG Dr Tedros and HRH Princess Muna al-Hussein open ICN-ICM-WHO Triad 2020 with focus on Nursing and Midwifery Workforces in the context of COVID-19
Collaboration with governments and need for psychosocial support for nurses, midwives amid COVID-19 pandemic
The ICN-WHO-ICM 8th Global Nursing and Midwifery Triad meetings were opened by WHO DG Dr Tedros Adhanom Ghebreyesus and HRH Princess Muna al-Hussein, WHO Patron for Nursing and Midwifery in the EMRO Region via live-link.
The meeting was chaired by Elizabeth Iro, WHO Chief Nursing Officer. Day One focused on Nursing and Midwifery Workforces in the context of the COVID-19 pandemic. The over 1200 registered participants viewed a special welcome video from the Steering Committee of Year of the Nurse and Midwife with messages from Dr Tedros; ICN President Annette Kennedy; ICM President Franka Cadée; Julietta Onabanjo, Regional Director, East and Southern Africa, UNFPA; and Lord Nigel Crisp and Professor Sheila Tlou, co-Chairs of Nursing Now.
Dr Tedros said: “It is essential that we remind our government that they invest in their nurses and midwives, that means jobs, education and leadership.”
Ms Kennedy emphasised: “This is not the International Year of the Nurse and Midwife that we had ever envisaged to showcase and celebrate nursing, but it has shown the great leadership of nursing…and that they are the backbone of the service. The State of the World’s Nursing report is a roadmap for the future, but we need to call on all governments to implement the recommendations. We also must work together to collaborate and share information.”
Lord Crisp added: “In the future, no one can surely doubt the professionalism of nurses and midwives or underestimate them.”
The participants were also welcomed by Triad Organizers: Jim Campbell, Director, Health Workforce, WHO; Howard Catton, ICN CEO; Sally Pairman, ICM CEO; and Anshu Banerjee, WHO Senior Advisor, Department of Reproductive Health and Research.
The opening address was given by HRH Princess Muna al-Hussein, WHO Patron for Nursing and Midwifery in the EMRO Region. She said “COVID-19 has illuminated the relentless efforts of nurse and midwives, jeopardizing their own and their families’ health for the care of all us.” She paid tribute to and remembered all the health workers who have given their lives during this pandemic.
“It is important to remember that employment in the health sector is an investment not a cost,” she said, adding that “never has that been truer than today. Health workers are currently keeping major economies from collapse.” She urged all government to give precedence to investing and empowering nursing and midwifery. “You have been and always will be my heroes,” she concluded.
Dr Tedros then gave opening remarks saying that, “The COVID-19 pandemic has put the global spotlight on nurses and midwives and the critical role you play…I would like to join Her Royal Highness to express how proud I am with all the nurses and midwives are doing giving or risking their lives to save others. We are proud of you.”
The first sessions of the day kicked off with a presentation by Dr. Socé Fall, Assistant Director-General, Emergency Response, WHO, who said that “health workers are the heartbeat that measures our hours”. Highlighting issues of PPE supplies and protection against violence and stigma, Dr Fall said that a whole society approach is required and that we must leverage human capital investment to bring lasting systemic change. “We invest in what we hold dear. We must invest in health workers,” he said.
The Presidents of NNAs in some of the hardest-hit countries provided their account of circumstances in their countries:
Walter de Caro, President of CNAI, the Italian Nurses National Association, said that the pandemic in Italy was like “a tsunami, like a war without a plan”. He spoke of the high price paid by health workers in Italy, with over 250 deaths, including 40 nurses who died from the virus and four who committed suicide. He stressed that there was a real mental health problem, but that there were also challenges related to PPE supplies, a lack of tests for health workers, shortage of personnel, and not enough beds or ventilators. Mr de Caro said there was a shortage of 50,000 nurses in Italy due to government cuts, but he also said the pandemic presented “a real opportunity for us: the public now know what nurses do, the importance of nurses as backbone of health system. During this year, the government decide to not invest and now we have to work for investment.”
Dr. Kyung-Rim Shin, President, Korean Nurses Association (KNA), spoke about the effective response to the virus in her country. She stressed the important role of KNA as a channel between the government and frontline nurses, saying “We are continuing close dialogue with the government and keep monitoring nurses’ needs”. KNA supplemented the shortage of nursing workforce and PPE; set up direct hotlines to provide counselling to nurses on the frontline and will continue cooperation with the government for legal rights and investment in nursing.
Hsiu-Hung Wang, President of the Taiwan Nurses Association (TWNA), also stressed the importance of government and workforce working together to quickly contain the pandemic. She was pleased to report that only four nurses in Taiwan had been infected and all have recovered. TWNA played a leadership and advocacy role, calling on government to cancel all large gatherings and advocating for supplies of PPE, and safe staffing levels. They worked throughout the outbreak to successfully enhance the professional image of nurses in Taiwan.
The importance of communication with the government was also highlighted by Dr José Luis Cobos Serrano, Deputy Secretary General of the Spanish General Council of Nursing (CGE). He said that, unfortunately in Spain, “communication with the government is often unreliable”. More than 60 health professionals in Spain had sadly died from the virus including five nurses, with care homes seeing the largest number of deaths. Dr Cobos Serrano said that Spain had a shortage off 100,000 nurses. “Preparation is key,” he said, “We need to approach any future pandemic prepared. We need to be able to stand with our patients 365 days a year and we will continue to do so.”
Perla Idolina Barragan Sosa, President of the Mexican College of Nurses (Colegio Nacional de Enfermeras), spoke about her country’s nursing shortages, which have been exacerbated during the pandemic, because so many nurses have become ill and unable to work. She also highlighted the terrible abuse and violence that some nurses had suffered in Mexico and the continuous support the College is receiving from ICN concerning 17 nurses who were kidnapped and robbed. “Yesterday we had a letter of support from ICN: it means we do not feel alone here in Mexico and we are most grateful to have this support. It has been very difficult here - our healthcare system has some weaknesses and we are still learning through the experience of the pandemic.” ICN President Annette Kennedy has sent a letter to the President of Mexico, urging an investigation into this latest very grave case and calling for justice.
Mohammed G. Alghamdi, President of the Saudi Nurses Association said the coronavirus is the greatest challenge that nurses in Saudi Arabia have ever faced. He said his government took the pandemic seriously early on, banning all international flights and even preventing travel to the holy site of Mecca to prevent infections. He added the number of nurses who became infected with the coronavirus was a concern that was addressed quickly. “28% of patients were healthcare professionals in the beginning. We worked collaboratively to bring the percentage down by being committed to all the international policies and protocols and making sure there was adherence to infection control protocols. The percentage of confirmed cases among healthcare workers is now less than 16%.” Mr Alghamdi also said Saudi Arabia is now working on plans to have a national nursing strategy to improve retention among nurses and a regional ‘surge capacity’ plan to help countries in the region to ensure they have enough nurses to manage pandemics in the future.
Thembeka Gwagwa, ICN Board member for Africa said the pandemic had put a strain on all countries but the effects were more serious in poorer countries like her own, South Africa. “It has also stimulated a robust debate worldwide between scientists and economists about what can be done to curb this ruthless and invisible enemy. We have managed to work together, to collaborate as people of the world, because we all know that, together we stand and divided we fall.” Ms Gwagwa thanked WHO and ICN for their guidance during the pandemic.
Dr Nonhlanhla Makhanya, Chief Nursing Officer, South Africa, told the meeting about the two major challenges that nurses faced in her country: the infection rate among nurses and human resources recruitment processes. “The infection rate in private and public sector is highest among nurses, and that is a cause for concern for us because it has implications for service delivery at various levels. We have also been having difficulty in recruiting specialist nurses in the surge period due to a chronic shortage.” She said that despite the government making more money available to employ more nurses, they were only being offered short-term contracts, which meant the jobs were not attracting many applicants. She also said nurses who had been redeployed to COVID-19 areas were often fearful, leading to high rates of absenteeism.
WHO, ICN and ICM each presented the work they have been undertaking to support nurses and midwives during the pandemic.
Gulin Gedik, Dept. of Health Systems Development, WHO EMRO said that “nurses and midwives have been involved and very instrumental in all stages of response to COVID-19”. She highlighted the challenges of increased workloads, high risk of infection, psychosocial impact, violence and stigma. WHO has developed tools to identify requirements of the health workforce and each country had developed technical guidelines to manage cases including other aspects of COVID-19 response such as contract tracing. She noted that infection among health workers is an important problem and that infection rates are not well recorded but said it was an average of 10% of cases but this can be up to 20% in some countries. She also spoke of the issue of mental health and wellbeing of health workers including burnout, stress and psychosocial issues. “In Canada, 47% of health workers expressed need for psychosocial support,” she said, adding that help lines are critical and that it is important to arrange working hours for adequate rest and recuperation times. She also added that it is critical to provide adequate transportation and accommodation to ensure health workers and their families are safe, and to ensure security to prevent violence against health workers.
Howard Catton, the CEO of the International Council of Nurses introduced ICN’s work including webinars in virtually every region to promote and share our learning: a 12-point call to action covering the key priorities, from PPE through to preparedness for future health system strengthening. He directed participants to the ICN COVID-19 portal for all ICN’s resources and links to WHO resources, as well as advice, stories and experiences from NNAs and frontline nurses.
Mr Catton made special mention of the need for systematic data on COVID-19 infection rates and deaths among HCWs, a call that ICN has been at the forefront of for many months. ICN data shows that the number of COVID-19 infections among nurses varies from less than 5% to up to 30%. “We believe the average health worker infection rate is probably around 7%,” he added. “We are in no doubt nurses are highest in terms of health worker infections.” 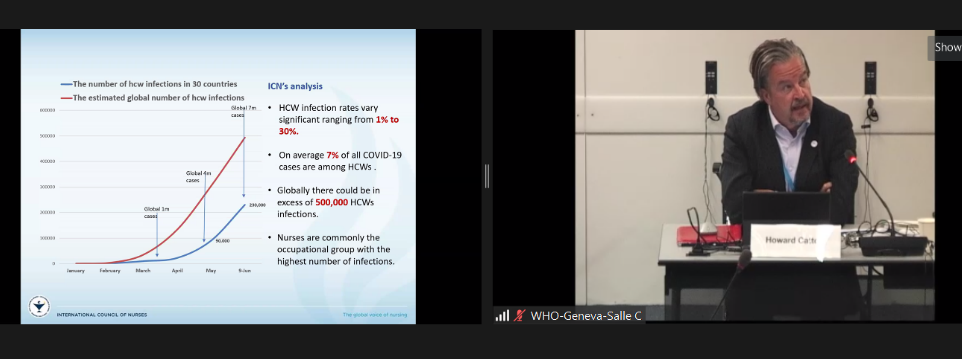
Mr Catton also spoke about the high number of deaths amongst nursing, particularly in Brazil, US, Mexico and UK. “It is a scandal that there is no official recording of infections and deaths amongst healthcare workers,” he said, calling for WHO to issue a clear recommendation for this information to be collected. “This is data that would help us to understand who is at risk and how we can reduce infection rates and save lives of nurses and other healthcare workers,” he said.
Mr Catton ended on a positive note, saying that this was a “phenomenal opportunity to advocate” and thanking ICN’s member association for helping to bring the experiences of frontline nurses to the headlines, providing “a bigger media platform than the International Year of the Nurse and Midwife would ever have done.”
Other speakers included: Florminda Tejano, Philippine League of Government and Private Midwives; Alison Eddy, CEO, New Zealand College of Midwives; Eun Suk PARK, Dept. of Infection Control, Severance Hospital, South Korea; Ann Yates, Lead Midwife Advisor, ICM and Inês Fronteira, GCNMO, Portugal; Stephane Okitokunda, Midwife, Kinshasha, Democratic Republic of Congo; Patricia Titulaer van Ham, ICM; Farah Babaey, Head of Midwifery Office, Ministry of Health and Medical Education, Islamic Republic of Iran.
Held virtually for the first time, the biennial meeting of Global Nursing and Midwifery Leaders will be held over the next three days with participants from the WHO regions of EURO, WPRO and SEARO joining in the morning and participants from AFRO, EMRO and PAHO joining in the afternoon.
To read the communique please click here.