Reviewing the world’s response to the COVID-19 pandemic
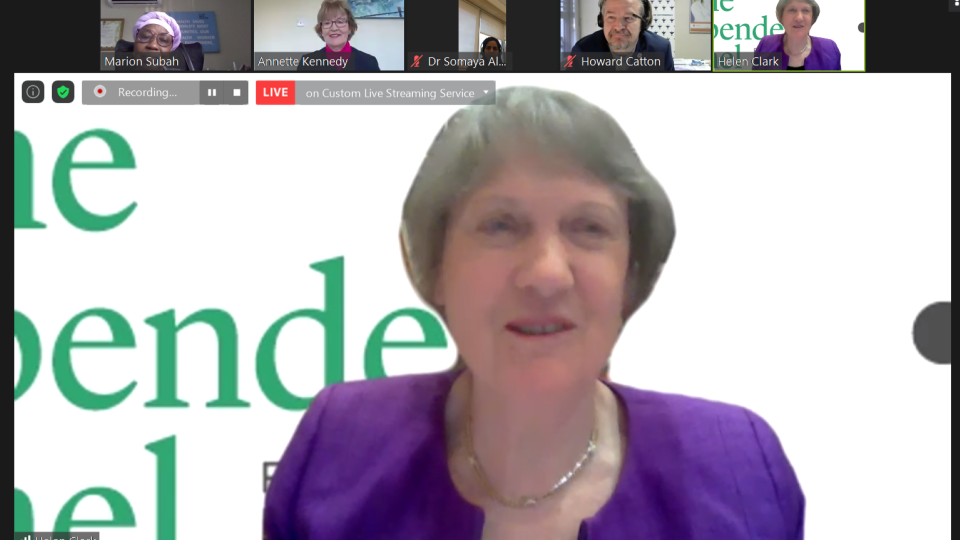
On 15 December 2020, the International Council of Nurses (ICN) and Nursing Now collaborated on a webinar to share nurses’ experiences of working on the frontlines of the COVID-19 pandemic.
The webinar, set up by the Co-Chair of the Independent Panel for Pandemic Preparedness and Response, former New Zealand prime minister the Rt Hon. Helen Clark, contributes to a review of the world’s response to the COVID-19 pandemic, including that of the World Health Organization.
The webinar was chaired by Marion Subah, Last Mile Health's Country Director in Liberia, and the panel consisted of Ms Clark, ICN President Annette Kennedy, ICN Chief Executive Officer Howard Catton and Nursing Now Executive Director Barbara Stillwell.
More than 250 nurses from around the world joined the webinar, and front-line nurses and National Nursing Association representatives from Ghana, India, Italy, Mexico, New Zealand, South Korea, Uganda, the United Arab Emirates and Zimbabwe, as well as members of the Nursing Now groups contributed directly during the discussion.
The main themes of the discussion included how well or poorly countries were prepared for the pandemic; the toll COVID-19 has had on nurses’ physical and mental wellbeing; immediate and long-term nurse staffing shortages and the terms and conditions that nurses are working under; the need to support and care for nurses; many of whom worked long hours and did not see their families for weeks; the abuse and violence nurses endured; and the need to make changes and involve nurses more in the development of healthcare systems of the future.
At the conclusion of the webinar, Ms Kennedy reflected on a number issues raised by participants which ICN has been highlighting since the beginning of the pandemic, including the stresses nurses have been under and the large number of nurses who are considering leaving the profession:
“We are very concerned about not having a workforce to look after the people, because without nurses in the workforce, there is no health workforce.”
Ms Kennedy stressed that nurses had provided strong leadership and found innovative ways to cope during the pandemic. As a largely female workforce, nurses’ contributions must be included in policymaking processes in the future, she said, rather than them just being expected to carry out whatever tasks they are asked to “without question”.
“I don’t think people have picked up the number of innovative things nurses have done during this pandemic, for example, training groups of doctors and nurses in caring for patients in the prone position and making changes that mean PPE lasts longer. Nurses are always trying to find innovative and creative solutions to deal with their problems, and I think that goes unrecognised. You have no idea how important it is for nurses to be heard” she said.
Ms Clark stressed is the need for policymakers to listen to what nurses have to say, and for nurses to be looked after, posing the question, “Who will care for the caregivers?”
She said the pandemic had exposed gaps in so many health systems, including shortages of personal protective equipment, that lead to threats to nurses’ health and wellbeing.
“One will never forget the images we saw on our media in some countries of nurses literally wearing garbage bags instead of protection, or of hearing of the need to wear the N95 masks multiple times. I am sure that the fact that there are simply not enough nurses in the world, a gap of millions of nurses, also leads to exhaustion and burnout, and those gaps also contribute in their way to illness and death.”
Mr Catton said that the webinar had provided a unique and powerful insight into the experiences of nurses during the pandemic in 2020.
“What is apparent from the webinar and the messages we have been hearing from our National Nurses Associations since the start of the pandemic, is that we need action and investment to support our under-pressure healthcare systems.
‘Participants articulated clearly that with the nursing shortage, it is not just the impact on the nursing workforce, it’s the impact on the safety and quality of care as well. Nursing must not disappear from the scene or be side lined when the pandemic is over. This spotlight that we have now needs to stay and nurses need to remain central to the design of health systems for the future. When Ms Clark brings her report to the World Health Assembly next year, ICN would want it to include indicators so that we know if we are making progress, so we never find ourselves waking up to a six million shortage, but we know whether or not we are doing enough and we need to act.”
ICN has called on governments to set up Health Education and Retraining Opportunity (HERO) funds to enable people, who have lost their jobs in the disruption caused to many industries by the pandemic, to train to become the registered nurses of the future.
Information from the webinar will contribute to a report that the Independent Panel for Pandemic Preparedness and Response will present to the WHO governing body, the World Health Assembly, in May 2021.
Any nurse who wants to contribute their experiences to the panel can do so here