ICN webinar focuses on central role of nurses in primary health care in achieving the goal of Universal Healthcare by 2030
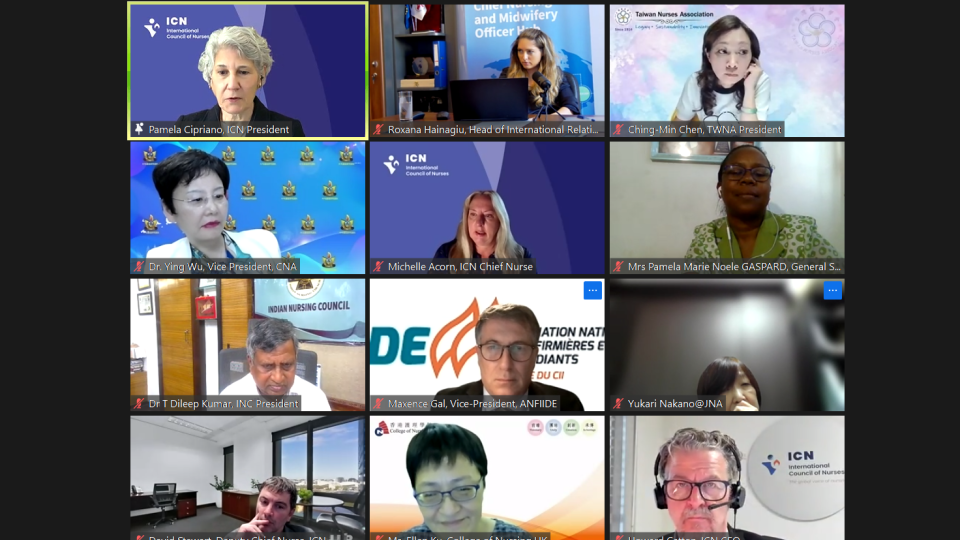
More than 300 nurses from over 100 countries attended the International Council of Nurses (ICN) latest webinar, which focused on the vital role of nurses in primary healthcare (PHC) in efforts to achieve the World Health Organization’s goal of Universal Health Coverage (UHC) by 2030.
ICN President Dr Pamela Cipriano, who moderated the webinar, spoke of the urgent need to provide healthcare for all, and said that the way to achieve it is to strengthen nursing in primary healthcare (PHC).
Message of support to nurses in conflict areas
Dr Cipriano and ICN Chief Executive Officer Howard Catton spoke about the current conflicts in the world, and their concerns for the many healthcare professionals who have been put in harm’s way while just doing their jobs.
Dr Cipriano said: “Our hearts go out to everyone affected. We condemn all violence and attacks on healthcare workers, hospitals and ambulance workers in conflict zones. We know that in many areas, whether it be in Ukraine, Israel, Gaza, Yemen, Afghanistan or Sudan over the past year, and certainly more intensely in the last few weeks, we continue to see the loss of human life and the sacrifices and the danger and risk for healthcare workers.”
She said ICN strongly supports the #NotATarget campaign and said ICN’s humanitarian fund and Nurses for Peace campaign are part of the call for peace around the world.
“We support all of our nurses on the front line and continuously are calling for respect for the international humanitarian and human rights laws to protect not only access to healthcare but healthcare workers and the safety of all civilians. We hope to see changes in our world that will keep people safe, whether they are caregivers or the people in our communities.”
ICN Chief Executive Officer Howard Catton said ICN had been contacted by nurses who were affected by the ongoing conflicts.
“We recognise their dedication and humanity. All the nurses we have contacted have been affected by personal loss and tragedies and are continuing to do their work to fulfil their professional responsibilities, while also dealing with grief and fear, and their own emotions. We have and will continue to recognise their courage, their dedication, their humanity, and the support from all of us as a global profession.”
ICN, PHC and UHC
Dr Cipriano spoke about ICN’s attendance at the United Nations High Level Meetings on healthcare in September and the central role that PHC plays in pandemic prevention, preparedness and response, the control of infectious diseases and UHC.
The political declarations that came out of those meetings emphasised that governments must take action.
“We are reinforcing the message that everyone must have access to care, and we must invest in primary healthcare because that is how we will be able to achieve the coverage that is needed.”
She laid out the principles of UHC:
- Everyone receives the care they need on a continuum from birth to death
- Care is of the appropriate quality to meet their needs
- It does not create financial hardship
She emphasized the necessity of having an effective, sufficiently skilled and properly funded healthcare workforce, which has been ICN’s consistent message at the recent high-level discussions.
Dr Cipriano is a member of the UHC 2030 Action Committee, which has reinforced the message to the United Nations and the World Health Organization that funding the healthcare workforce is not a cost but an investment.
“When countries invest in health they invest in their people, and that strengthens their preparedness for any kind of disasters and affects their ability to have a robust workforce: and when people are working, we have healthier economies.
‘Now is the time to amplify our messages about how important it is to invest in nursing and take advantage of the drivers of change. That can be everything from digital disruption to addressing our workforce, to recognizing that person-centred care is fundamental to how nurses look at our communities and the people we serve. we know that nurses provide better value, particularly with our advanced practice workforce. “
She spoke about the need for investment in nursing leadership and innovation to provide the mentorship that nurses need in a rapidly changing world, and the need for continuing education across the globe.
“This is a really important time for all of us when you think about the opportunity for nurses to do more in the delivery of primary healthcare as we are on our journey towards Universal Health Coverage. Taking advantage of the advances in healthcare, and that’s everything from digital technologies to working with our patients so that they are informed. Addressing the workforce challenges has been at the top of our list now for the last couple of years. We must be able to get the investments of our governments so that we can reduce the workload and have more individuals able to provide care. And we need to have more leaders who are speaking to our authorities and elected officials to get the resources that we need.“
Dr Cipriano ended by saying the UHC is the place where nurses can have the most impact on people’s lives and ensure that health systems are robust and able to deliver the care that is needed.
ICN’s continuing support for nurses in PHC
Mr Catton gave an overview of the effects the pandemic had on the world’s journey toward UHC and gave a history of ICN’s interventions on the topic since the Alma-Ata declaration in 1978.
“That declaration signalled the shift from a hospitalised and medical approach to primary healthcare based public health approach, the importance of people within the context of their communities, respecting their rights, integrating their healthcare and ensuring equity in provision as well.”
He spoke about ICN’s role over the years in advancing nurse education and developing nursing roles, and the importance of recognising the social determinants of health, and that nursing is “the very essence” of PHC.
Mr Catton said primary care is the gateway to the health system for many people, and nurses are a vital workforce for achieving UHC, largely through their work in PHC. ICN has been working to inform WHO, its governing body the World Health Assembly and its regional offices, of the importance of the nursing workforce in meeting their aims.
“People get the fact that PHC is the road to UHC, but they don’t necessarily then join the dots to nurses as the people who will carry us along that road to our destination, and that is important for us to continue to do. We have been thrown off track by the pandemic. It has exposed a lack of preparedness and increased inequalities. If we remain committed to our ambition of Universal Health Coverage for all we simply are not going to do that without investing in our nursing workforce.”
He said ICN’s 2023 Charter for Change included the need to enable nurses to work to their full scope of practice and for health systems to be reorientated toward home-based and people-centred care.
Mr Catton said the next State of the World’s Nursing report, which ICN is working on, would inform the next WHO Strategic Directions for Nursing and Midwifery, and that this would provide an opportunity to put nurses’ roles in primary healthcare to the fore.
He said a new PHC publication that ICN is finalising, will include information from the webinar.
ICN Deputy Chief Nurse David Stewart
ICN’s Deputy Chief Nurse David Stewart gave a presentation about how the health workforce could develop to meet the needs of UHC through PHC.
He highlighted workforce shortages, not just among nurses but medical staff, especially family doctors, poor access to care and investigations, non-involvement of patients in decisions about their care, and that many healthcare staff are employed in roles that do not acknowledge or make the most of their skills and experience. Mr Stewart said although there was little data on patient safety in primary care, what has been captured is very concerning.
Mr Stewart said: “Four in ten patients are harmed in primary and outpatient healthcare. Five per cent of adults in high-income countries experience diagnostic errors leading to potential harm and there are five million deaths in low and middle-income countries due to poor quality care. Almost half of people in OECD countries have poor coordination of their care, and about 10% of medicines are fake or falsified.”
Mr Stewart said nurses can make a real difference to all of this, especially in the roles of care coordinator, nurse navigator or case manager.
One example where they can make a real difference is in helping so-called ‘frequent flyers,’ who are a small group of people who account for between 25 and 40% of emergency department (ED) attendances.
Attending to the needs of such patients, who often have chronic long-term healthcare conditions in primary care, avoids unnecessary ED attendance and admissions to hospital.
Mr Stewart said: “Some studies suggest that for every dollar spent on care coordination or nurse navigation, there is a five dollar return on investment.”
He said the traditional model of PHC is more often focused on communicable diseases, short interventions and little or no follow up. But as the disease pattern has changed to more chronic conditions, there is a need for longer consultations and a multidisciplinary team approach.
“There is a desire to move towards a more comprehensive model, where the patient is more in charge of their own health and wellbeing, with a whole multidisciplinary team with multi-sector collaboration. When this model has been implemented, there are significant benefits: for example, in Costa Rica there was an 8% reduction in presentations in EDs, and there was an increased satisfaction rate among each of the providers. A similar phenomenon was found when it was implemented in team-based care in Canada where, when it was implemented in relation to respiratory and other viral infections, productivity of the multidisciplinary team improved by 26%.”
Mr Stewart said the answer to many of the issues in PHC can be addressed by reimagining the delivery of PHC in different settings.
ICN Chief Nurse Michelle Acorn
ICN Chief Nurse Michelle Acorn spoke about the range of different models of care that there are in PHC, including nurses working in clinics, concentrating on noncommunicable diseases such as diabetes, and working in their own communities to improve health outcomes and tailor interventions based on their community’s needs.
Dr Acorn mentioned that nurses work in many different environments including schools, prisons and hospices, as well as in people’s homes. And that they focus on many aspects of care including targeting risk factors for disease reduction, promoting healthy lifestyles, and playing key roles in preventative measures, such as vaccination programmes, supporting independence, health counselling, health promotion, and early detection and screening for particular diseases.
She said problems in recruitment of PHC staff often means payments are increased leading to care becoming unaffordable and creating access issues and a two-tiered system.
Dr Acorn said the appointment of specialist nurses can help to resolve these problems.
“In the US the current ratio of physicians to advanced practice registered nurses is two to one, and it is expected to shift to one to one by 2032. Nurses offer workforce solutions in primary healthcare. The marginalised and poor are often left without care. Advanced practice nurses, like nurse practitioners and clinical nurse specialists enhance healthcare and are proven to safely and effectively improve healthcare access.”
Dr Acorn said one particular area of practice that nurses can make a real difference in is prescribing.
“When we talk about prescriptive authority for nurses, we know that they are safe and effective, there is rigorous education and training to ensure safe prescription practices and there are evidence-based approaches to medication management. And nurse prescribing improvs efficiency by reducing wait times and streamlining care delivery. If a nurse can’t prescribe, it can lead to a break in care continuity and patients may face delays in receiving necessary treatment.
‘Nurses have the knowledge, competence, expertise and leadership to accelerate progress towards Universal Health Coverage and optimising access to primary healthcare if we invest, progress and monitor implementation of primary healthcare.”
Dr Acorn recommended that nurses access ICN’s free education modules on Patient Safety and the WHO’s Global Strategic Directions for Nursing and Midwifery.
Input from Representatives from ICN National Nurses Associations
Kerri Nuku, Kaiwhakahaere (Governance leader), New Zealand Nurses Association
Ms Nuku said primary healthcare and universal healthcare are the keys to ensuring equitable services to New Zealand’s population and communities.
Ms Nuku said: “Our organisation has realised that as a small island country we have gone through some significant traumas over the last year with the impact of Cyclone Gabriel. We have never had disasters as such and it has required us to rethink the way that we plan our care, to rethink the way that we practise.
‘Our organisation has developed a strategic plan called Maranga Mai! It is a comprehensive strategy that does a number of things. It looks to allow nurses to take the lead and make some political decisions to ensure that nursing voices aren’t silent at the table where decisions are made. That there is an ability for nurses to collectively influence health outcomes by being part of the policy decision makers.
‘That is a significant shift because for many years our nurses have felt that they have not been proactive enough to make those decisions. One of our strategic plans is to ensure that we have nurses everywhere standing up. That is the meaning of Maranga Mai! – to stand up and take action collectively beside primary healthcare, community and the hospital sector. We have also developed strategies that will look at indigenous health and wellbeing, so that alongside any policies that we are making or are involved in, we critically apply a cultural lens to ensure that no indigenous population is left behind and that the voices of Māori and of Pacifica, who are always overrepresented in poor health outcomes, are never far from policy decisions.
‘We have had significant impact due to the natural disasters. It has made us look at how we critically involve communities in decision making. What we found is that decisions are made further away from consumers, so involving them in decision making, connecting up again with nurses, ensuring our equality lens is applied to everything we do, is part of what we have got to make as natural and normal.
Yukari NAKANO, Executive Director, Japanese Nurses Association
Ms Nakano said: “Japan is recognised as an early achiever in Universal Health Coverage and at the same time, it is the leading country in terms of challenges.
‘The rapid population ageing with a declining birth rate is causing a significant impact on health issues in terms of both quantity and quality. At the same time, it is causing institutional challenges about how the system can be sustained.
‘With such recognition Japan has been promoting healthcare policies for about a decade against a rapid increase in the elderly population, aiming at 2025 when the ageing problem will become quantitatively more serious. Around the same time the Japanese Nurses Association published Vision for the Future of Nursing for 2025, taking the roles of nursing in protecting the health, life and dignity of all people living in the community from both the medical and life perspectives of nurses.
‘Over the past ten years we have been working to achieve this vision through better education, practice and leadership development, and expanding the fields of nursing and stimulating activities in local communities.
‘After 2040, when the elderly population will reach its peak we will not only see further declining birthrate and population decline, but also qualitative changes in the elderly population. The challenges we must address will become even more serious. The JNA is currently working on a new vision based on the discussion on the social issues in the 2040s as well as on guidelines for initiatives after 2025.
‘Healthcare systems in Japan have focused on responding to diseases after they have appeared, and a large amount of social security funds and healthcare resources have been invested in treatment. On the other hand, resources for health promotion and disease prevention are not sufficient. The health of people in the community will be more important in the future and we hope to create nursing activities that fulfil the primary healthcare functions.
‘Such enhanced primary healthcare by nurses will contribute to the efficient use of healthcare resources. We strongly emphasise that without nurses in primary healthcare, UHC can never be achieved.”
Dr Ying Wu, Vice President, Chinese Nurses Association
Dr Wu said: “China has a high internet penetration rate as well as social media. The WeChat social media platform has more than 1.3 billion active users across the country. WeChat is more than just social media – it has become an indispensable part of daily life for the majority of Chinese people.
‘It also offers features like mini programmes which provide an extra platform for applications. As a result, nurses and nursing researchers have harnessed the capabilities of WeChat and WeChat mini programmes to conduct health and patient management.“
Dr Wu said there have been thousands of papers published by nurses about their use of WeChat in patient care. Such initiatives have significantly contributed to the achievement of UHC.
Dr Wu said one example enables patients with noncommunicable diseases to remotely monitor their condition and risk factors, report their symptoms and the app then provides appropriate interventions.
“This approach reduces the incidence of ischaemia events, ER visits, hospitalisation and mortality.”
She said she is currently working on Artificial Intelligence-enhanced digital nursing, with the aim of making UHC a reality as soon as possible.
Maxence Gal, Vice President ANFIIDE (France)
Mr Gal said: “In France primary health care does not depend on a hierarchy and the thing is that we still don’t use it that much because the definition is still too wide. It is also because since 2009 we have had the Hospital, Patient, Health and Territory Law, and unfortunately, that means that physicians are the key professionals. What is more, we have understood nowadays that nurses are key, and the pandemic has reshaped everything, and today the legal framework is evolving and now they understand in parliament that changes are needed.
‘We are taking part in the development of new care models where nurses can contribute more to efforts throughout our country. We support a new organisation, in line with the government’s objective stemming from a new law from 2016. As a consequence we are working with old practices, with new protocols and with a new funding law of 2018.
‘We understand that today nurses have a lot of potential that they can help people and they are to be invested in for community care. Our body has been identified by the ministry of healthcare to work on nursing and today we promote competences, good practices in line with the needs of citizens, we work on training and so on.
‘We are also deeply involved in prevention at the primary level with inoculation, with WHO. We also work at the second level with chronic diseases and on the third level with prevention. Our organisation is also deeply involved in France in other activities in order to widen the activities nurses can carry out, mainly when it comes to cancer care.
‘We have been working with patients for many years and have a true partnership with French organisations representing patients, and we defend patients’ rights as well. We have a proactive policy to widen the care of citizens.”
Pamela Marie Noele GASPARD, General Secretary, Mauritius Nurses Association
Ms Gaspard said 40% of the human resources for healthcare are nurses and midwives, and the public health services in Mauritius are designed to achieve universal health coverage.
They provide services in 18 area health centres, 116 community health centres, five mini clinics and two community hospitals.
“Despite the remarkable things we have accomplished, Mauritius faces many challenges, which include the growing burden of noncommunicable diseases, the complex health needs of the ageing population and the rising expectations of patents for more patient-centred and improved quality of care.
‘The Mauritius Nursing Association has played an important role in influencing policy and has collaborated with the government in the development of the Health Sector Strategic Plan. While building on the health gains already achieved, the strategic plan unveils concrete strategies and interventions to address major health challenges in the country, and people’s expectations for an enhanced quality of service across their lifespan. It provides a coherent framework that will guide policy makers, stakeholders and partners in health development over the next five years.
‘The strategic plan proposes a comprehensive set of actions to re-engineer and revamp our health delivery services in the light of an emphasis on customer care, enhancement of primary care, health promotion, preventive medicine and specialised services.
‘Nurses play an important role in Mauritius in achieving the strategic actions, which include encouragement of early detection of breast cancer and cancers of the female reproductive organs, to increase access to screening services at the primary healthcare and community levels, the scaling up of HPV vaccination coverage among adolescent girls, the setting up of menopause clinics in gynaecological and obstetric departments in all hospitals.
‘Strengthening our nurses among targeted groups of the population including the consequences of backstreet abortion and its adverse effects, undertaking screening for early detection of intimate partner violence, and making hospitals and other healthcare centres more user friendly.
‘The future of nursing relies on effective use of population data to plan the nursing workforce. In Mauritius there is an acute shortage of staff. There is also a need for specialise education at the post-registration level, and digital health still remains a key challenge.”
Ching-Min Chen, President, Taiwanese Nurses Association
Ms Chen spoke about her government’s setting up of a health insurance system for its 23 million citizens in 1995. At that time it covered only half of the Taiwanese population, but she was pleased to say that now it covers almost 100% of the people.
Ms Chen said: “In addition our government has initiated three investments and six actions in nursing since 2018, intending to strengthen our primary healthcare and ultimately to help fulfil the goals of UHC, which includes investing in home health nursing, effective nursing and asthma nursing.
‘The six actions are: to reimburse the nursing service in long-term care payment; initiate community based family nurse practitioners to serve in remote areas; invest in nurse leaders to serve as advisory committee members at the national health research institute, in order to make health and nursing policies; implement an advanced practice registered nurse accreditation system; establish telehealth care services in remote areas, and monitor the national nursing workforce.
Roxana Hainagiu, Head of International Relations, The Romanian Order of Nurses and Midwives
Ms Hainagiu described some key strategies that Romania has put into action for the reform its primary healthcare.
“First, prioritising screening and prevention, which centres around increasing the focus on screening and prevention at the primary level. We firmly believe that prevention is not only the most cost effective, it also leads to better patient outcomes. And we have provided incentives for primary care practitioners including nurses to actively participate in prevention programmes, encouraging them to take on a more active role in the overall health of our citizens.
‘Our second key strategy entails substantial efforts to improve the infrastructure and capabilities of primary healthcare facilities. We have increased renumeration mechanisms for primary care cabinets, which includes both physicians and nurses, to make them more attractive. Additionally, we have launched an investment programme that has equipped 3,000 primary health practices with modern equipment.
‘Nevertheless, it’s not solely about infrastructure, so we are challenging healthcare professionals to step or of their comfort zones, encouraging them to expand their roles and prescription rights, and to embrace a more proactive and holistic approach to healthcare.
‘We remain committed to working closely with the Ministry of Health of Romania to expand the roles of nurses and midwives in delivering improved healthcare to our communities. Community based care often serves as the first point of contact for patients and by employing nurses in this role we can guarantee improved health outcomes for all.
‘We have revised the payment mechanisms for nurses, along with doctors practising in rural areas to make these areas more appealing to healthcare providers, and recently our regional conference, organised with the support of the WHO office in Romania, along with local stakeholders and experts, to concentrate our efforts on empowering nurses to provide care at the community level.
‘Additionally, we must adapt to a whole new landscape of care by addressing digital health innovations. We have invested in systems in this area in Romania. And we invested in integrated database for better evidence-based policies for the health workforce.
‘We are very proud to be at the forefront of a comprehensive consultation that has concluded with a political resolution framework for action on the healthcare workforce in the WHO European Region. This resolution is an essential step towards implementation of an agreement from earlier this year.”
Dr T Dileep Kumar, President, Indian Nursing Council
Dr Kumar spoke about how the Indian Nursing Council is working toward Universal Health Coverage by 2030, to which he said the government of India had given a high priority.
“All 150,000 subcentres, which cater to a population of five to ten thousand people, have been converted into health and wellness centres. They are having a very important component of nursing by positioning the nurse as a community health officer. These community health officers are all graduate nurses. To enable us to have more community health officers, we have taken the policy decision to integrate their training into the existing BSc curriculum, which is being converted into a competency-based programme to improve the quality of nursing education.”
Dr Kumar said his organisation has established a state-of-the-art simulation centre to train faculty members at Master’s level, so that they would be able to deliver the new competency-based programme.
“The nurse practitioner programme has been approved by the government of India and the Indian Nursing Council in collaboration with the Ministry of Health. It has been estimated that 84,000 nurse practitioners will need to be trained.”
Dr Kumar said leadership is also an important issue in India, and the council hosting the ICN Leadership for Change to train 40 Indian nurses.
The new Nursing and Midwifery Commission will take decisions about how the nurses’ scope of practice will be implemented in India.
“This will go a long way towards providing nurses and midwives to achieve universal health coverage.”
Ms Ellen Ku, President, College of Nursing, Hong Kong
Ms Ku said there are a number of PHC project that are ongoing in Hong Kong.
“In 2018 the Hong Kong Department of Health produced a document, Towards 2025: Strategy and Action plan for Prevention and Control of NCDs. It’s about public education, opportunity to promote healthy living.
‘In 2019 we had the launch of the first district health centre, with the expectation that each district will have a community health so that people won’t have to go to hospital, and start to introduce the concept of primary healthcare, and putting it into action. With this in hand, the government established a primary healthcare office under the health bureau, and then a primary healthcare blueprint was published in 2022.
‘I am going to talk to the commissioner of the primary healthcare office because the patient booklet says PHC is about having a ‘family doctor for all’. I am going to propose it should be a ‘family doctor and nurse for all’. That will be the concept.
‘One of the items the government wants to address is healthy Hong Kong, which has different categories for all walks of life, from reproduction to the elderly services. One key message is we bring health services to the community and promote ageing people in the city. There are a lot of new ideas and perspectives in this area. It is a challenge for the healthcare system and for nurses, most of their training right now is based on the traditional model, and not much about primary healthcare, so nurses are not well prepared. We are talking about a revamp of the education curriculum.
‘Since there is a shortage of nurses. Because of the promotion of healthy life in the community there is another stream of education development to have healthcare workers. They are trained but they are not going to practise as nurses. They are going to take up part of the work in the community. I don’t know if that is a threat or if there will be advantages for nurse in Hong Kong.”
Ms Ku said there have been changes to the legislation that will make it easier for overseas nurses to work in Hong Kong. The challenges nurses face include technological developments and bringing the electronic healthcare record to all areas of Hong Kong.
She ended by saying that there are a lot of opportunities for nurses to learn in Hong Kong and invited nurses from around the world to visit Hong Kong’s nurses to speak more about PHC.
Concluding remarks
Dr Cipriano acknowledged the work being done by nurses around the world in promoting PHC.
She ended the webinars by saying: “We must invest in our people; we must invest in healthcare. We consistently find that nations are behind in meeting those targets, but it doesn’t mean that we stop pushing. So both in our Charter for Change and the political declarations coming out of the United Nations, particularly about UHC2030, it is about high level commitment and investment and action.
‘Similarly our discussions about the roles of nurses – one of our questions was about how do we stop premature deaths from noncommunicable diseases – these are the fundamental places where nurses makes a difference and where ICN has focused on providing resources. We encourage you to use all of the resources at your disposal from ICN, and we will continue to make this a significant focus as we continue to focus on our Charter for Change to shore up our workforce and overall investments. We will make sure we are linking health security to UHC, to the role of nurses in primary care and to the outcome of health for all. We will play a significant role [in this] together.”